Senator Welch Joins Fight to Block Pilot Program Using AI Decision-Making in Traditional Medicare
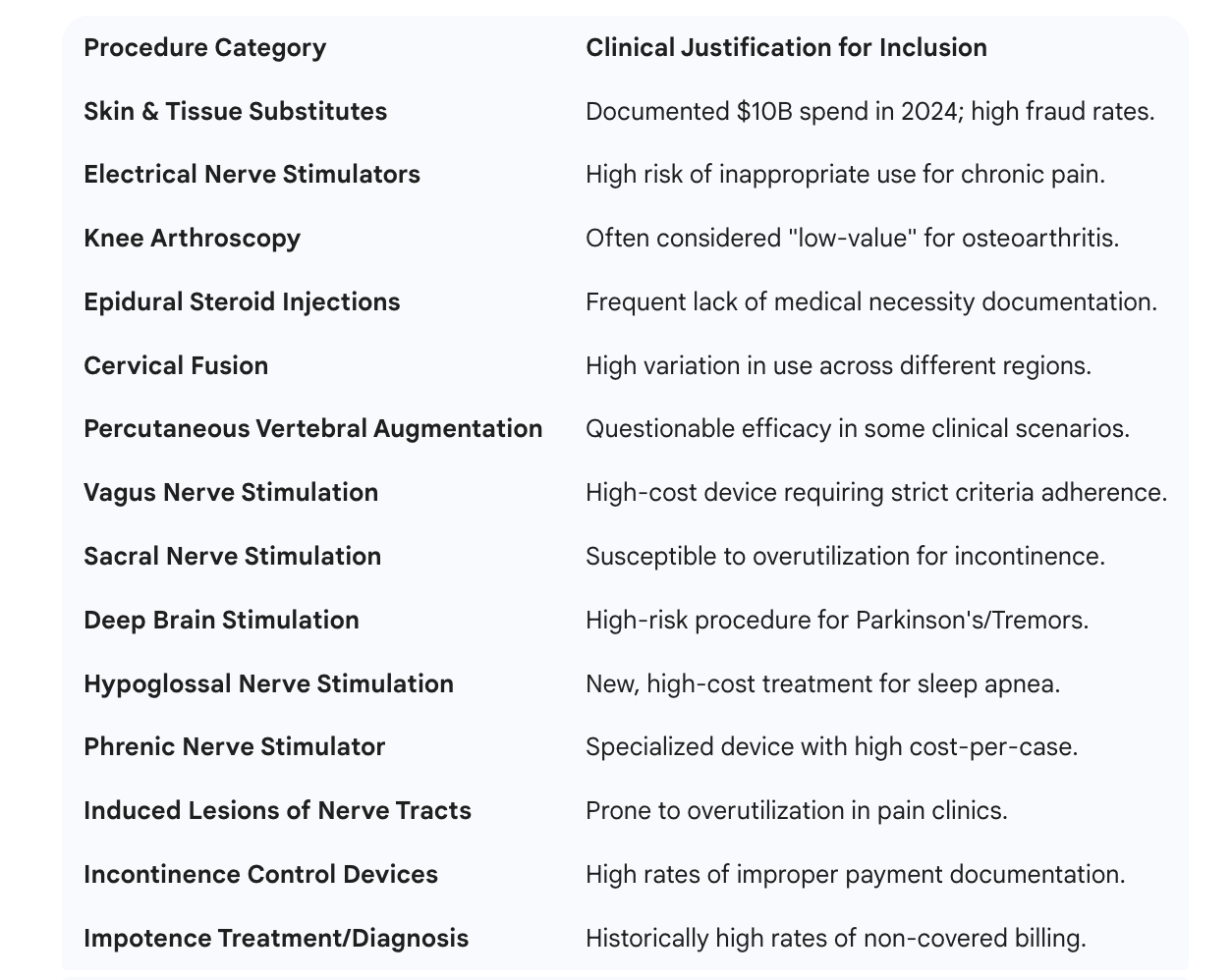
The pilot targets a specific subset of 14 primary procedures (encompassing 23 regulatory standards) that CMS has identified as having high rates of “low-value” use or fraudulent billing.
Senator Peter Welch (D-VT) has joined a bicameral coalition of lawmakers to introduce the Seniors Deserve SMARTER Care Act, a legislative move aimed at halting the implementation of a new artificial intelligence-driven pilot program in Traditional Medicare.
Welch’s opposition centers on protecting Vermont’s seniors and rural healthcare providers from what he describes as “burdensome red tape” and “roadblocks” that allow profit-driven algorithms to override the medical judgment of doctors.
“From Day One, the Trump Administration has been on a rampage to wreck Medicare and make health care unaffordable,” Welch stated. “Their newest plan to let AI take over important Medicare prior authorization decisions will be a disaster for providers and make it harder for seniors to get the care they need.”
For Vermont, a state where roughly 67% of Medicare beneficiaries choose Traditional Medicare specifically to avoid the restrictive hurdles of private plans, the stakes of this federal pilot are uniquely high.
The WISeR Model: Importing Private-Sector Rules
The program Welch is fighting, the Wasteful and Inappropriate Service Reduction (WISeR) model, is a six-year pilot scheduled to begin on January 1, 2026. Created by the Centers for Medicare & Medicaid Services (CMS), it seeks to import “prior authorization” strategies from the private sector—specifically Medicare Advantage—into Traditional Medicare.
Under the current system, Traditional Medicare typically pays for services first and audits for fraud later. The WISeR model reverses this, requiring doctors to get approval before performing specific procedures. The goal is to curb fraud, particularly in the skin substitute market, which saw over $10 billion in spending in 2024—much of it deemed wasteful by federal watchdogs.
How the AI Functions
The WISeR model uses six technology firms to manage these approvals using AI and machine learning:
Automated Screening: AI compares doctor requests against Medicare’s evidence-based rules.
Auto-Approval: Clear-cut cases can be approved almost instantly by the software.
Human Safeguard: CMS mandates that any denial (non-affirmation) must be reviewed by a human clinician. AI cannot deny care on its own.
The “WISeR 14”: Procedures Under Scrutiny
The pilot targets a specific subset of 14 primary procedures (encompassing 23 regulatory standards) that CMS has identified as having high rates of “low-value” use or fraudulent billing.
Why Senator Welch and Others Are Concerned
The primary objection raised by the Seniors Deserve SMARTER Care Act is the incentive structure of the pilot. The private tech companies are paid a share of “averted expenditures”—essentially, they receive a commission on the money saved by denying or reducing care.
Welch and his colleagues argue this creates a “perverse incentive” to deny care that may be medically necessary. Furthermore, they highlight the impact on Vermont’s rural health system:
Administrative Burden: Small Vermont practices often lack the staff to manage complex new authorization portals.
Automation Bias: There are concerns that human reviewers, pressured by quotas, may simply agree with AI flags rather than performing a thorough clinical review.
What Happens Next?
The WISeR model is set to go live in six pilot states on January 1, 2026. While Vermont is not in the first wave, the results will determine if this becomes the new national standard for all Traditional Medicare beneficiaries.
The Seniors Deserve SMARTER Care Act is currently moving through the House and Senate. If Welch and his colleagues are successful in passing the bill, the WISeR model will be prohibited before it can begin. If not, Vermont providers will likely spend 2026 watching the pilot states closely to prepare for a potential nationwide rollout.