Armed with Bad Data: Vermont Regulator Wages War on Gifford Hospital
Vermont's Green Mountain Care Board continues to prioritize standardized billing data in order to support their policy goals even after receiving the more reliable clinical reality.
The Big Picture
Gifford Health Care in Randolph stands at a crossroads. A state-commissioned report has recommended potentially drastic changes to this community hospital, including the possible closure of its inpatient beds and birthing center.
Hospital leaders, however, have identified significant errors in the data used to make those recommendations—errors they say fundamentally misrepresent how busy and essential their facility actually is.
This situation matters to every Vermonter living in or near the White River Valley. The outcome will shape whether families can deliver babies close to home, whether patients can be admitted for observation overnight, and whether the region will have reliable access to emergency care.
What Led to This Point
In 2022, the Vermont Legislature passed Act 167, a law acknowledging that healthcare spending in Vermont was growing faster than the economy while rural access was shrinking. The law directed the Green Mountain Care Board—the state’s healthcare regulator—to study how hospitals could be reorganized to control costs and improve care.
The Board hired Oliver Wyman Life Sciences, a global consulting firm, to conduct a comprehensive review. The consultants spent over a year analyzing data and interviewing stakeholders. Their final report, released in September 2024, identified five major challenges facing Vermont’s health system: rising costs, hospital financial losses, an aging population, long wait times, and health disparities between rural and urban areas.
What the Report Recommends for Gifford
The Oliver Wyman report suggests that hospitals like Gifford should consider converting to a “Rural Emergency Hospital” or “Community Ambulatory Care Center.” These federal designations, described in state materials, allow facilities to provide emergency and outpatient services while eliminating overnight inpatient beds.
For Gifford, this would mean ending the ability to admit patients overnight for conditions like pneumonia or heart problems, closing the labor and delivery unit, and focusing on stabilizing patients before transferring them to larger hospitals like Dartmouth Hitchcock Medical Center or the University of Vermont Medical Center.
The Data Dispute
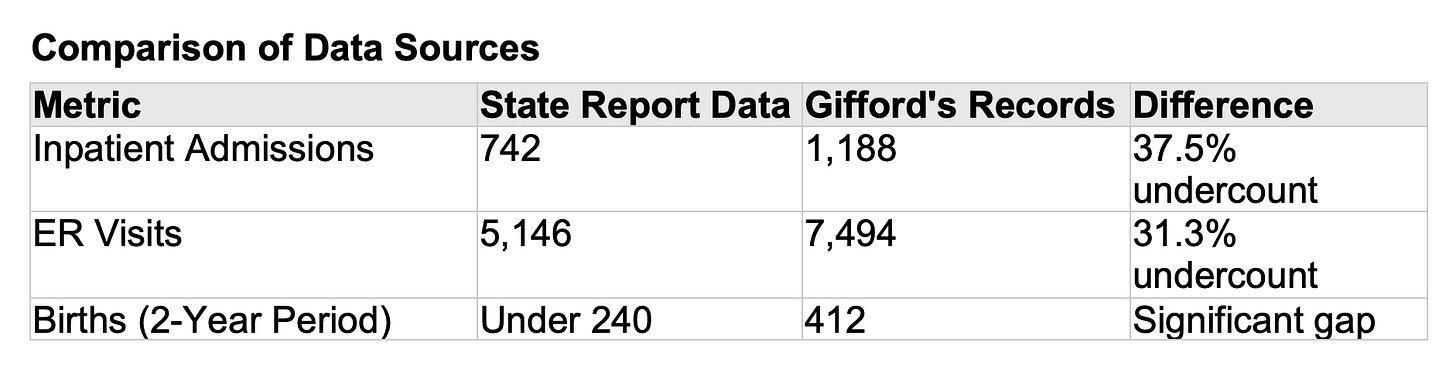
After reviewing the Oliver Wyman report, Gifford’s leadership conducted an internal audit that revealed substantial discrepancies between the state’s data and the hospital’s own records.
The birth numbers carry particular significance. Clinical guidelines often suggest that obstetric units with fewer than 200 births per year may struggle to maintain staff proficiency. According to the state’s figures, Gifford appeared to fall below that threshold. According to Gifford’s own data, the hospital averages over 200 births annually, meeting the safety standard.
Why the discrepancy? Such gaps often arise from how data is counted. State databases typically rely on billing claims, which may exclude patients classified as “observation” rather than “admitted,” or may miss self-pay patients and those covered by out-of-state insurers.
The Financial Reality
While the volume data is disputed, Gifford’s financial struggles are not. The hospital reported operating losses exceeding $10 million in the most recent fiscal year. State data shows Gifford’s operating margin fell from negative 8.3% in 2023 to negative 18.2% in 2024.
Several factors drive these losses. The post-pandemic nursing shortage forced hospitals across Vermont to hire expensive traveling nurses. Reimbursement rates, regulated by the state, haven’t kept pace with inflation. And running a 24/7 emergency room, operating room, and birthing center requires a baseline of staff whether the units are full or half-empty.
Meanwhile, the University of Vermont Medical Center—Vermont’s largest hospital—posted a surplus of over $60 million during the same period. This contrast raises questions about how the current healthcare system distributes resources between urban academic centers and rural community hospitals.
New Leadership, New Strategy
In October 2024, Gifford’s board appointed Michael Costa as President and CEO. Costa brings an unusual background: he previously served as Deputy Commissioner of Vermont’s Department of Vermont Health Access (the state Medicaid agency) and as Deputy Director of Health Care Reform for Vermont. He also led Northern Counties Health Care, a federally qualified health center in the Northeast Kingdom.
Costa’s response to the Oliver Wyman report has emphasized transparency. In November 2024, over 300 community members packed Judd Hall Gym in Randolph Center for a public forum on the hospital’s future. Costa described the state’s recommendations as “concerning” and “shocking” while asking the community to “stand by us.”
The hospital’s strategy has pivoted in an unexpected direction. Rather than viewing Gifford as a facility that sends patients to larger hospitals, leadership is positioning it as a “relief valve” for overwhelmed academic medical centers. With UVM Medical Center reporting a 3,000-patient waitlist for colonoscopies, Gifford has established transfer agreements to accept patients from Dartmouth and UVM. This fills empty beds with insured patients while easing pressure on the larger hospitals.
Difficult Choices Already Made
While fighting to preserve core services, Gifford has made cuts to demonstrate fiscal responsibility. In November 2024, the hospital announced the immediate closure of its chiropractic and urogynecology services. These specialty services were likely operating at a loss, and eliminating them allowed leadership to prioritize the emergency department, primary care, and birthing center.
The hospital has also worked to reduce its dependence on expensive traveling nurses. International recruitment has brought new staff, including an operating room nurse from Colombia through a partnership with an overseas nursing recruitment firm.
A Region Losing Services
Gifford’s situation unfolds against a backdrop of regional service cuts. Central Vermont Medical Center in Berlin closed its inpatient psychiatric unit. Rutland Regional Medical Center closed its pediatric inpatient beds. Copley Hospital in Morrisville announced it would close its birthing center, citing annual losses of $3 million to $5 million and projecting fewer than 120 births per year.
Each closure shifts pressure elsewhere. Psychiatric patients now board in emergency rooms across the region. If both Copley and Gifford close their birthing centers, a large swath of central and northern Vermont would become what healthcare advocates call a “maternity desert”—an area where expectant mothers face drives of 45 minutes or more to reach delivery services.
A Looming Threat: The 2026 Insurance Cliff
Beyond the immediate hospital restructuring debate, a federal policy change could destabilize healthcare economics across Vermont. The American Rescue Plan Act provided enhanced subsidies that cap health insurance premiums at 8.5% of household income for all Affordable Care Act enrollees, regardless of income.
These enhanced subsidies are set to expire at the end of 2025 unless Congress extends them. If they lapse, families earning more than 400% of the federal poverty level—roughly $124,000 for a family of four—would lose all federal help with premiums. Some analysts project that monthly premiums for such families could jump to $2,500 or more.
If that happens, some families may drop coverage entirely. When uninsured patients need emergency care, hospitals often cannot collect payment. For a facility like Gifford already operating at a loss, even a modest shift in its payer mix toward uninsured patients could prove devastating.
Key Questions Remain Unanswered
The dispute between Gifford and the state hinges on whose numbers are correct. If the Oliver Wyman report relied on flawed data, then recommendations built on that foundation may not apply to Gifford’s actual situation. The state has not yet publicly addressed the discrepancies Gifford has identified.
There is also the question of capacity. The Oliver Wyman approach assumes that patients currently served by rural hospitals can be absorbed by larger academic centers. But if those centers already have 3,000-patient waitlists for routine procedures, closing rural inpatient beds could create new bottlenecks rather than efficiencies.
Finally, Vermont must weigh financial sustainability against geographic access. Rural hospitals are expensive to operate because their fixed costs are spread across smaller populations. But closing them imposes costs of a different kind: longer drives, delayed care, and the loss of an economic anchor in small communities.
What Happens Next
The Green Mountain Care Board will continue its review of Vermont’s hospital system under the Act 167 process. Community engagement sessions are ongoing, and the Board is expected to issue further guidance on hospital restructuring in 2025.
Gifford’s leadership has made clear it intends to fight for its current service lines, particularly the birthing center. The hospital’s strategy of positioning itself as overflow capacity for academic centers will be tested in the coming months as transfer agreements take effect.
The legislature will also play a role. Lawmakers may revisit hospital funding formulas, address the data discrepancy concerns raised by Gifford, or take action on the looming insurance subsidy cliff at the federal level through advocacy.
For residents of the White River Valley, the outcome will determine what healthcare looks like in their community for years to come. Whether Gifford remains a full-service community hospital, converts to an outpatient-focused model, or finds some middle path will depend on how regulators, hospital leaders, and the community navigate the months ahead.




I don’t use the ESV for these very reasons, preaching out of the NIV (which is also our pew Bible). My daily reader is the 2020 NASB, & I also appreciate the CSB & NET.